My Philosophy
If you’re here, you already know breast cancer isn’t just about your diagnosis.
It changes your body, your mind, your relationships — and your sense of safety.
Yet the system you’ve been navigating was built to treat disease, not guide you back to yourself.
This page names what’s missing in survivorship care — and offers a different way forward: a practical, body-based approach that puts your whole self back at the center.
You’re not failing at breast cancer survivorship. You’re navigating it without a map.
Survivorship isn’t the end of your breast cancer story — it’s the rest of your life.
And you deserve to live it with confidence, clarity, and the skills to take care of yourself in ways that actually work for your body.
Most people are sent out of treatment with a stack of discharge papers, a few follow-up appointments, and the quiet hope that time will take care of the rest. But real healing doesn’t just happen because the calendar moves forward.
What’s missing in most survivorship care?
A practical, body-based approach that makes you more self-sufficient, not more dependent.
That’s what my work is about: giving you relevant, realistic tools to reconnect with your body, manage the ongoing impacts of breast cancer, and finally feel at home in yourself again.
If you’ve ever thought, “Why didn’t anyone tell me this part?” — you’re in the right place.
On this page, you’ll find:
Why survivorship can feel harder than anyone prepares you for,
The Six Fundamentals that create a real foundation for healing,
How my work brings them together so you can move from surviving to truly living.
You were handed a set of false expectations and promised a finish line that feels more like a revolving door.
Why Survivorship Feels So Hard
No one prepares you for what it’s actually like to live with breast cancer. Not just the diagnosis. Not just the treatment. But the whole experience.
From day one, the focus is narrow: Kill the cancer. Manage the side effects. Stay on schedule.
What’s left out?
The human experience of cancer — your safety, your identity, your mental and emotional well-being.
Here’s the truth:
The medical system is built to treat disease. It isn’t built to help you feel safe in your body again, make sense of the emotional fallout, or learn how to care for yourself in the years that follow.
So if you’ve been feeling lost, second-guessing every ache or twinge, smiling and saying “I’m fine” when you’re not — it’s not because you’re doing survivorship wrong.
It’s because you’ve been asked to navigate it without a map.
There is no standard of care for life in survivorship. We are each left to create our own, on our own.
Why Healing Can Feel So Disconnected
That missing map doesn’t just leave you feeling unprepared — it impacts every part of your healing.
Here’s how I see it show up again and again:
No space to slow down — Rest feels like failure. Guilt pushes you to keep going.
No context for what’s normal — You’re left guessing, Googling, and second-guessing every sensation.
Piecemeal professional care — No one’s talking to each other, and you’re left to connect the dots.
Generic self-care — You try the things… but they weren’t made for your body or your history.
An unclear sense of self — You’re not who you were, but you don’t yet know who you are now.
A lack of true community — Support groups feel too heavy or too pink, while friends and family can’t relate.
When only a few of these areas get minimal attention, you get just enough relief to keep going — but not enough to truly move forward.
The result?
Survivorship becomes a silent, disjointed slog — leaving you disconnected from your own body, unsure of what’s working, and quietly afraid of what’s not.
Over time, this “new normal” can mean:
A shoulder that gets tighter until your favorite activities are out of reach.
Swelling in your arm that creeps in and suddenly becomes chronic lymphedema.
Scar tissue that binds and restricts movement, left untreated because it’s not “urgent.”
Constant second-guessing, decision paralysis about food or exercise, and brain fog from unprocessed stress.
A deep loneliness, guilt, and the inability to fully trust your body again.
Time alone doesn’t fix these things — and more often, they quietly get worse.
If this sounds familiar, know that there’s a way to address all of it — and it starts with the Six Fundamentals below.
Recovery might happen on its own, but to really heal you need to be an active participant.
The Six Essentials Every Survivor and Thriver Deserves
Through both my professional work and personal experience, I’ve learned that these gaps aren’t random — they’re predictable. And when you address them intentionally, everything changes.
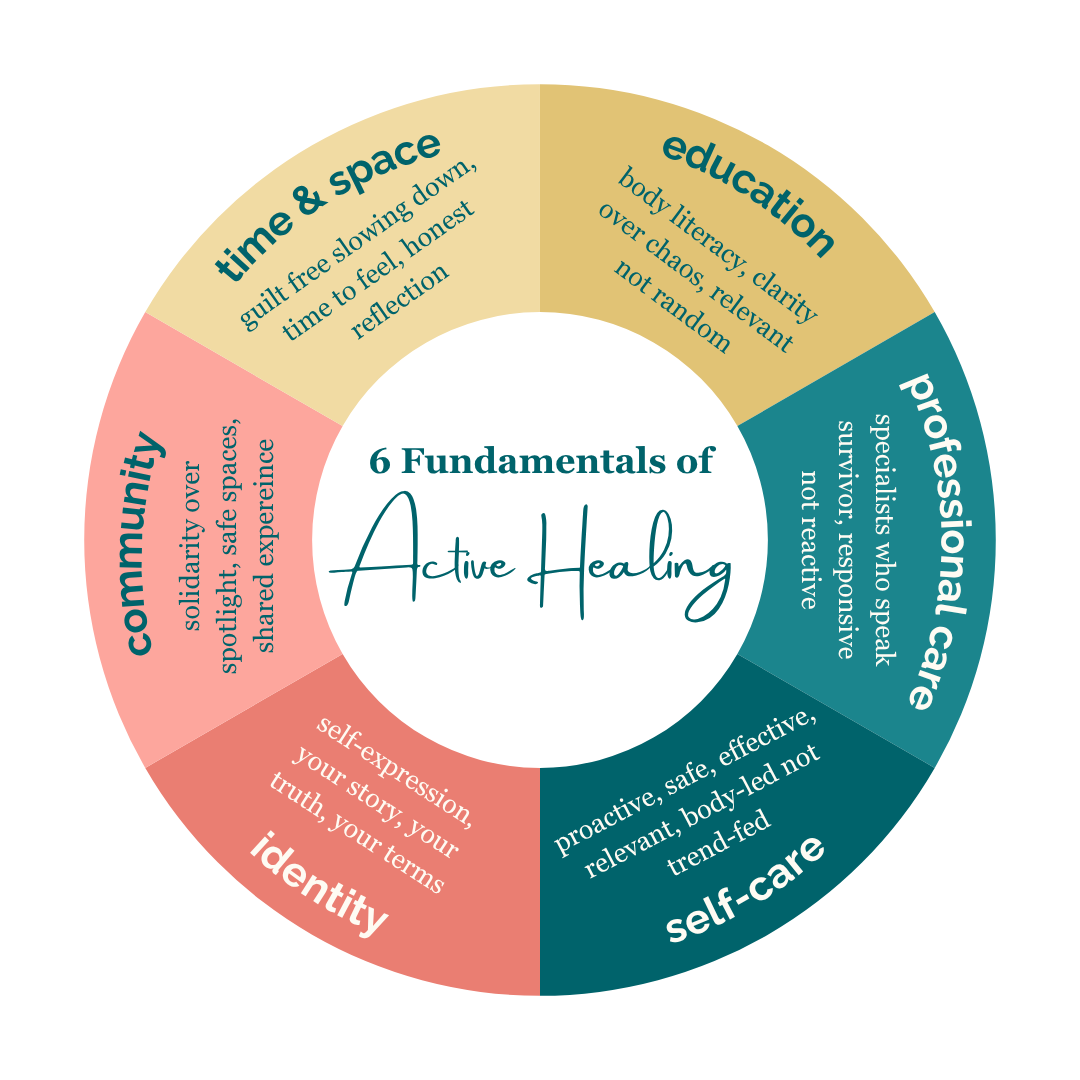
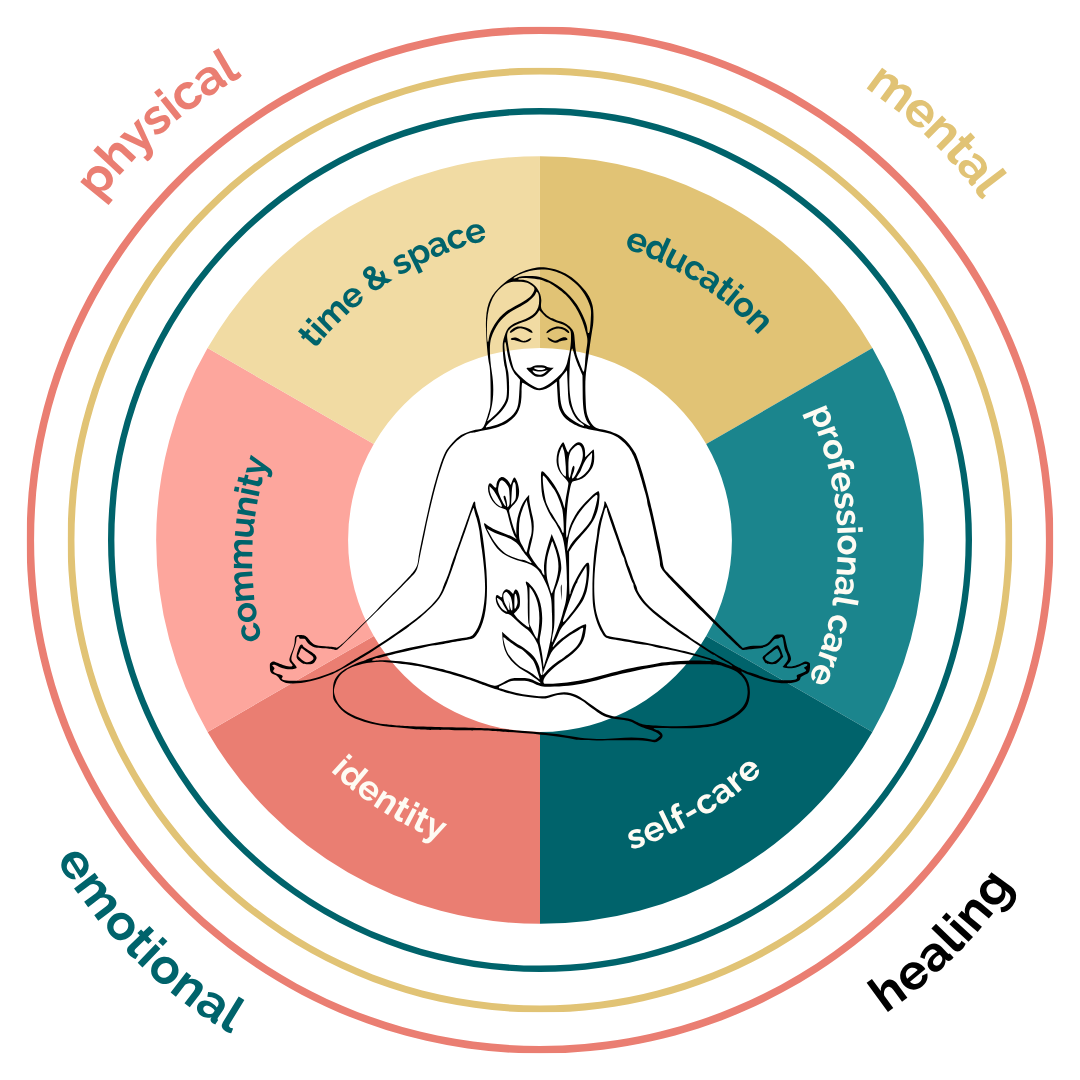
That’s why my approach is built on Six Fundamentals that support your whole self:
Time & Space — Creating the physical, mental, and emotional room for healing to actually happen.
Context & Education — Understanding what’s normal, what’s not, and how to respond with confidence.
Professional Care — Connecting the right providers so you’re supported, not scattered.
Self-Care — Tailoring practices to your body, your history, and your current reality.
Identity — Exploring who you are now, beyond diagnosis, and reclaiming your sense of self.
Community — Finding the right people who truly understand — without the overwhelm or pressure.
When these six elements work together, you move from piecing things together on your own to having a clear, compassionate roadmap for your recovery.
Survivorship care needs to be rooted in relevance and real-life functionality, not aspirational habits.
Healing after breast cancer isn’t about doing more — it’s about doing what matters.
You don’t need to move out of your body. You need a safe, effective way to move back in.
I’m not here to “fix” you or hand you a list of shoulds.
I’m here to give you the skills, context, and confidence to take care of yourself in ways that actually help — so you can stop guessing and start living.
My work is about turning the Six Fundamentals into everyday tools you can actually use — not just ideas that sound good on paper.
Whether we work together 1:1, in a group program, or you prefer to do it on your own through my free and on-demand resources, everything I share is:
Relevant — rooted in your real life, not generic advice.
Realistic — doable within your energy, time, and capacity.
Restorative — helping you feel more at home in your body, day by day.
Body-based — because healing is physical and everything else.
Evidence-informed — grounded in what we know works for breast cancer survivors.
Compassion-driven — because survivorship is hard enough without judgment.
Because healing isn’t about “getting back” to who you were — it’s about becoming someone who can live fully now, with the body and life you have today.
How I Work
You don’t need to move out of your body. You need a safe and effective way to move back in.
This is the Healing You Deserve.
This is what healing really looks like — not bouncing back, but integrating forward.
It’s not about doing more. It’s about doing what matters.
And when you begin to come home to your body, here’s what I see—again and again:
The pain softens.
The range of motion returns.
The fear quiets.
The questions (and answers) become clearer.
The scar tissue becomes something you can work with—not against.
You stop bracing for the next thing to go wrong.
You begin to trust your body and yourself again.
And that changes everything.
As Your Breast Cancer Self-Care Specialist, my job isn’t to hand you a list of rules or ask you to depend on me forever.
It’s to walk with you—at first—so that you can eventually walk with more confidence on your own.
I believe the best healing support helps you become more informed, more connected, and more self-sufficient—not more reliant.
That’s what this work is about. That’s what self-care actually looks like. And that’s where we begin.
Ways I Can Support You
Oncology Massage & Lymphatic Drainage
Located in Buffalo, NY, I exclusively serve the breast cancer community with gentle, safe, and specialized care for real, hands-on relief.
Ask Amy Virtual Consultations
If you’re feeling stuck or unsure what to do next, a one-time virtual consultation might be exactly what you need. We’ll talk through your situation and create a plan that works for you.
DIY On-Demand Self-Care Solutions
Practical, body-based digital resources like e-books and workshops that give you real tools to support your healing—on your own terms, at your own pace.